Older people may have a range of dietary needs. People with diabetes who are well and have a good appetite can enjoy a balanced healthy diet (refer to section on Eatwell Guide).
Many older people living with diabetes are more likely to have support needs and/or health conditions that impact on their food and drink intake e.g. weight loss, swallowing problems which may require texture modified diets, low mood, depression and dementia. This makes it more important to ensure that food and drink provided is enjoyable, nutritious and accessible, in order to maintain their health and wellbeing.
- Regular meals, drinks and snacks (if needed) provide a structure to the day
- Making sure they are hydrated is essential. Provide and encourage regular fluid intake throughout the day e.g. water, tea, coffee, low calorie /no added sugar squash cordials and soft drinks e.g. diet/zero etc
Foods are no longer able to be labelled as diabetic or suitable for diabetics, they may be labelled as ‘reduced sugar’ or ‘No added sugar’ which can be used as part of a balanced diet, (see section on food labelling).
Balancing Nutritional Requirements throughout the Day
Eating healthily can be enjoyed by everyone. Healthy eating when someone has diabetes is the same as healthy eating for people without diabetes. Food and nutrition, alongside medication when required and activity, is the cornerstone to diabetes management. People with diabetes should be able to continue to enjoy a wide variety of foods.
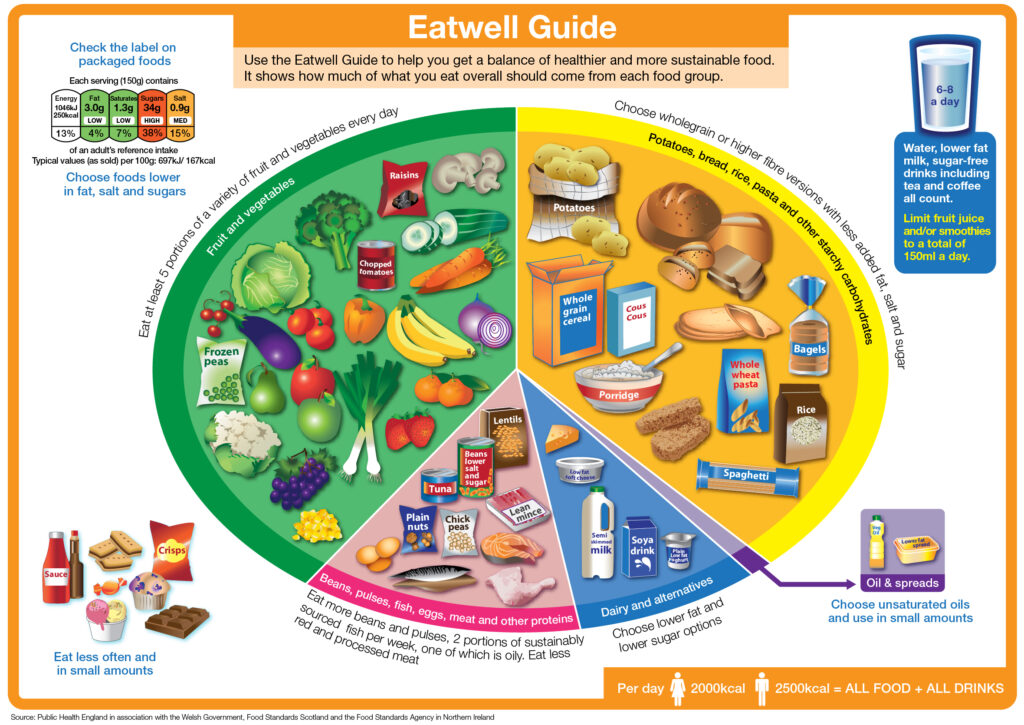
The Eatwell Guide is used across the UK to help everyone understand what the ideal balance of foods is for a healthy diet and is aimed at children over the age of 5, adolescents, adults and older people in good health. It promotes a healthy balanced diet with lots of fruit and vegetables, high fibre cereals and grains, lower fat, sugar and salt in order to help prevent many conditions that are linked to a poor diet.
How much and what types of food to have during the day
For those with a good appetite the Eatwell Guide encourages us to choose a variety of foods from the 5 food groups to help us get the wide range of nutrients our bodies need to stay healthy.
Those with a poor appetite may find smaller, more frequent meals and snacks easier to manage. It may be necessary to have a different balance of these food groups, including more of the high calorie foods. Please refer to the section below for MUST screening and managing the risk of undernutrition. If you need further support, please contact the local Nutrition & Dietetic service.
The five food groups are:
- Potatoes, bread, rice, pasta and other starchy foods
- Fruit and vegetables
- Beans, pulses, fish, eggs, meat and other proteins
- Dairy and alternatives
- Oils and spreads
If you work in a care home there is lots of useful information about nutrition and hydration needs and how to plan meals for residents including those with diabetes – Please refer to the Welsh Government’s Food and Nutrition in Care Homes for older people – Best Practise Guidance, available on the link: Food and nutrition guidance for older people in care homes | GOV.WALES.
Potatoes, bread, rice, pasta and other starchy foods (contain starchy carbohydrates)
1-2 portions per meal – depending on body weight and physical activity. Try to include wholegrain versions when possible.
A portion is equal to 2 – 3 tablespoons of breakfast cereal; 1 slice of bread; 2-3 tablespoons cooked rice, pasta, mashed potatoes; 2 new potatoes; 2-3 crackers/crisp breads; 5 – 8 chips.
Fruit and vegetables
They are packed with vitamins, minerals and fibre. Aim to offer at least 5 portions daily. A portion is 2-3 tablespoons vegetables or 1 piece of fruit e.g. 1 apple/pear/orange/handful of grapes/level tablespoon of dried fruit/small glass of fruit juice.
All fruits are allowed, and all contain slow releasing natural sugars.
Beans, pulses, fish, eggs, meat and other non-dairy sources of protein
They are important for the repair of the body’s muscles and can help to maintain muscle mass and so reduce the risk of frailty. Aim for 2 – 3 portions daily.
A portion is: 2 – 3oz (50-80g) red meat, chicken; 4 – 5oz (120-150g) fish; 2 eggs; small tin of beans/3 tablespoons of pulses/lentils.
Dairy and alternatives
This group is important for bone health, and apart from cheese contains natural sugars which are slow releasing. Aim for 3 portions every day.
A portion is: 1/3-pint milk; Small pot of yoghurt/ fromage frais; 2 tablespoons cottage cheese; 1½ oz (30g) cheese (small matchbox size); small portion of custard (150mls).
Oils & Spreads
A portion is 1 – 2 teaspoons oil/ margarine/butter.

Foods and drinks high in fat and/or sugar
This includes products such as chocolate, cakes, biscuits, full-sugar soft drinks, butter and ice-cream. These foods are not needed in the diet and so, if included, should only be done infrequently and in small amounts. Food and drinks high in fat and sugar contain lots of energy, particularly when eaten as large servings. These maybe included if the resident has been identified at risk of malnutrition (refer to nutrition care plan).
A portion is 1 – 2 teaspoons mayonnaise/salad dressing; 1 scoop ice cream/1 tablespoon cream;1 mini chocolate bar/chocolate biscuit; Small packet of crisps; 2 teaspoons sugar/jam/ honey.
Which foods affect blood glucose levels?
All carbohydrate foods break down into glucose, which in turn affect blood glucose levels. These include the starchy carbohydrates (the bread, potato, rice group); the ‘added’ sugars from the fats and sugars group; and the natural sugars from milk and fruit. Having a healthy, balanced diet helps with both weight management and blood glucose control.
Practical note:
Starchy foods should, make up about a third of the daily diet
• Provide 1-2 portions of foods from the starchy food group at every meal and some as snacks (when appropriate)
• Include wholegrain and high fibre options
• If blood glucose levels are high, consider overall portions and quantity of carbohydrate foods & drinks NOT just high sugar foods
Nutritional Care for People with Diabetes who are at Risk of Malnutrition
All Care Home residents and older adults cared for at home should be screened on a monthly basis to identify their risk of malnutrition and to ensure appropriate care plans are in place. MUST is the validated screening tool for screening across Wales.
For those identified as medium or high risk – a ‘food first” approach should be taken and if high risk consider referral to the dietitian.
Strategies to follow:
Malnutrition Universal Screening Tool (MUST)
MUST score 0: Low Risk
Practical note: Obesity
It can be very difficult to people to lose weight in a care home setting especially if less mobile. Empathy and understanding are key, raising the issue sensitively and explaining the benefits of some weight loss can help. Regular physical activity (dependant on ability) combined with modest reduction in calories can help to either maintain weight or achieve small weight loss. Offer low sugar/no added sugar drinks, this is an easy way to reduce overall carbohydrate intake.
MUST Score 1 – Medium Risk
Repeat screening after one month:
- If score improved, continue regime for a further month, then gradually reduce food fortification.
- If no change or deterioration, consider specialist treatment below.
- If deterioration, follow HIGH RISK nutrition care plan
- Oral health risk assessment
- Provide/implement Good Food First advice
- Provide snacks between meals and homemade nutritious drinks
- Ensure any assistance required for eating and drinking is provided
- Ensure any recommendations regarding food and fluid texture modification are followed and any specific advice for eating or drinking is followed i.e. position when eating for swallow
- Weigh weekly (if unable to weigh use MUAC – Mid Upper Arm Circumference).
- Use food and fluid charts to record food and drink intake for 3 days. In residential settings use the All Wales Food and Daily and weekly intake and output charts
MUST Score 2 or more – HIGH RISK
If no improvement, consider below:
Refer to your local dietetic department for more detailed assessment and advice.
Follow local guidance or request prescription of oral nutritional supplements (ONS), e.g. 2 per day for 4 – 12 weeks*.
Please note these supplements will not be suitable for patients with chronic kidney disease (CKD) stages 4 & 5).
Practical Tips to support people with diabetes & risk of malnutrition:
- Plan for three regular meals a day. Try to help avoid skipping meals and space breakfast, lunch and evening meal over the day. This will not only help control appetite but also help in controlling blood glucose levels
- Include starchy carbohydrate at each meal: the amount eaten is important to manage glucose levels
- Offer high protein snacks such as cheese & biscuits and/or nourishing drinks e.g. milk
- If glucose levels are raised DO NOT STOP oral nutritional supplements, if prescribed
- Speak to the GP or Dietitian

Frequently Asked Questions
Undertaking regular MUST screening will identify individuals at risk of malnutrition. There are a number of measures in place for those identified as medium risk. Please consider asking the G.P. to refer to the local dietetics department for assessment and advice if an individual is at higher risk. If able, monitor blood glucose levels to avoid hypoglycaemia, especially in those taking medications such as gliclazide and insulin. Request a review by the community diabetes nurses or G.P. if blood glucose levels become low or very high.
Request advice from the G.P. who may refer to speech and language therapy for a swallow assessment. A texture modified diet and or thickened fluids may be required for people having swallowing difficulties. This will help them manage food and drinks safely. Care/Nursing Homes should refer to the IDDSI description for modified texture – refer to Food and nutrition guidance for older people in care home l GOV.WALES. https://gov.wales/food-and-nutrition-guidance-older-people-care-homes
If you are a carer, escalate to the nurse in charge (if in a care/nursing home) first. Request an urgent review by the community diabetes nurses or G.P.
Some individuals may experience taste fatigue if prescribed nutritional supplements for a long period of time. There are a range of nutritional supplements available and ways in which you can provide a variety of suitable nutritious drinks or snacks. If they are under the care of the community dietitian, request a review and further advice, otherwise speak to the G.P.
Healthy older people with diabetes who are not at risk of malnutrition do not always require additional snacks and can often enjoy a healthy balanced diet containing regular meals. Smaller more frequent meals or additional snacks/supper may be required for some individuals, such as those who have a reduced appetite or intake, and those at risk of malnutrition or are taking certain medications.
Yes, a healthy diet can include some sugar and is not considered a sugar free diet. There are natural sugars found in fruit and dairy products and these foods provide vitamins, minerals and fibre too. Limit added sugars from foods such as cakes, biscuits, chocolate and sugary drinks. These foods can increase glucose levels and may cause unnecessary weight gain if eaten in larger amounts. If the person living with diabetes has been identified at risk of malnutrition, foods higher in sugar may be included as part of their nutritional care plan.
A good balance of a variety of both fruit and vegetables can be included each day. However, eating large amounts of fruit in one sitting may cause high blood glucose levels. To avoid higher glucose levels, for the person living with diabetes they should be encouraged to eat one portion of fruit at a time and spread other portions eaten across the day.
Foods are no longer able to labelled as diabetic or suitable for diabetics, they may be labelled as ‘No added sugar’ which can be used as part of a balanced diet (see section on food labelling). A smaller amount of regular chocolate or jam can be used. If the person with diabetes has been identified at risk of malnutrition, foods higher in sugar may be included as part of their nutritional care plan.
Sweeteners don’t affect blood glucose levels and are often used as an alternative to sugar. They can be included if residents prefer to use them.
Puddings or deserts provide additional carbohydrate to a meal which may be required if a patient has a small appetite or is at risk of malnutrition. If a person with diabetes is eating well and not at risk of malnutrition, puddings or deserts may increase blood glucose levels and cause unnecessary weight gain. Encourage them to make healthier pudding choices or offer smaller portions less often. It is not necessary to make separate puddings made with sweeteners for people living with diabetes.
It can sometimes be difficult to approach visitors who like to bring their relatives additional food and drinks. Many visitors are often unaware that certain foods or drinks can affect diabetes and cause high glucose levels. If able, speak to the family/visitors and offer some ideas for alternatives or perhaps ideas for non-food and drink items that would be enjoyed, such as a magazine or some flowers.
Any activity that encourages able people with diabetes to move around more and spend less time sitting is of benefit. Encourage able people to walk to the dining or recreational areas for meals and activities, or outside to spend time in garden area (if available).