Managing Hypos?
Please access the following PocketMedic film Managing Hypos
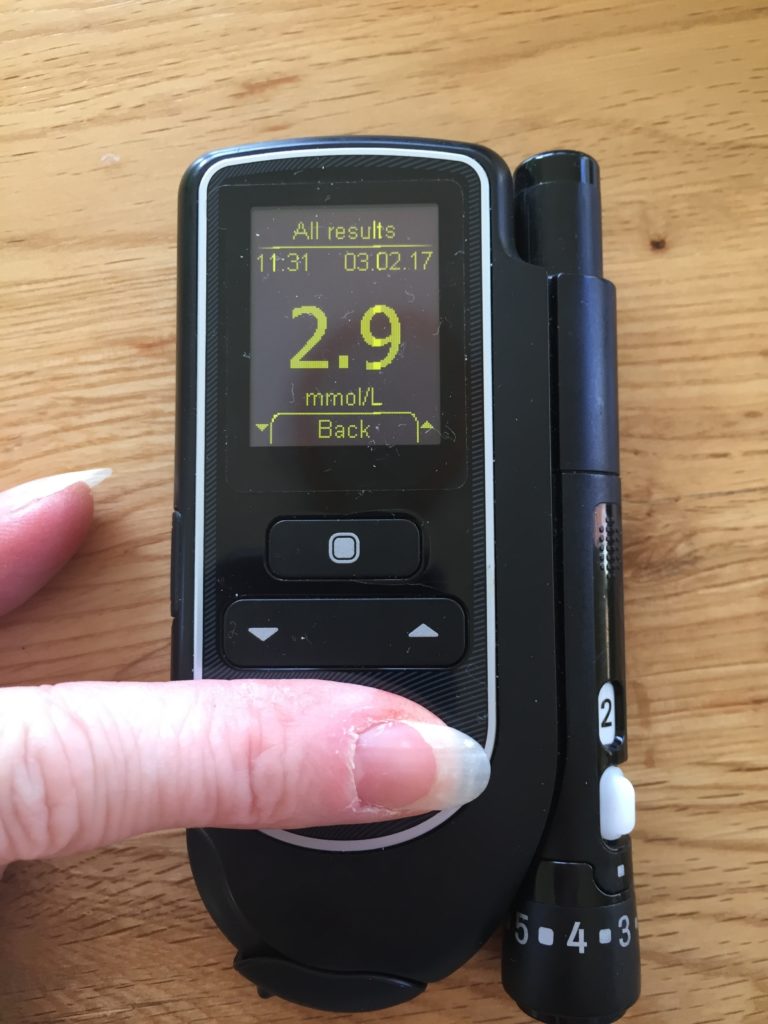
Hypoglycaemia (hypo – low glucose levels)
This is a blood glucose level of less than 4.0 mmol/l and should always be treated with fast acting glucose to prevent complications such as a fall; worsening of other conditions; fitting or collapse.
Why is this important?
Your brain needs glucose to function. If the glucose level drops it will affect behaviour. People may not always be able to explain their symptoms and tell you they are having a ‘hypo’ so they may need to have their glucose target set at a higher range to reduce their risk of having a hypo.
Hypoglycaemia may lead to:
- falls
- arrhythmias or angina/chest pain,
- fitting and coma if not managed quickly and appropriately
A change in behaviour or in how they ‘look’ should alert you that their glucose levels may be dropping. The priority is to ensure the person with diabetes is safe, and the target glucose range should be individualised and documented as part of their care plan.
Who is at risk of having a hypo?
People with diabetes on insulin therapy and/or tablets e.g. gliclazide:
- who may have lost their hypo awareness signs
- who have had recent changes in medications
- who have a poor appetite or change in diet/feeding regime (may be a new resident who is having difficulty in settling and those refusing to eat or unable to eat)
- who are currently unwell
- who have kidney disease
- who have heart disease
- who have liver disease
- of advancing age or mental health issues (who may be unable to communicate they are having symptoms)
Hypo Unawareness
Some people may have no symptoms or they may not be able to tell you they have symptoms and so it may be down to you as their carer to be observant. If you suspect that someone you care for may be unaware they have symptoms, inform the GP or usual health care professional.
Anyone needing insulin or certain glucose-lowering tablets called Sulphonylureas (e.g.
- gliclazide
- glimepiride
- glibenclamide
- glipizide or glinides (e.g. repaglinide)
have a higher risk of hypoglycaemia particularly if their usual meal pattern is altered through acute illness or nausea. It is important to be aware of who may be at risk of having a ‘hypo’ so that you can try to prevent it from happening.
It can be quite alarming for a person having a hypoglycaemic event and it can also be scary witnessing a hypoglycaemic episode. Therefore, knowing the signs and symptoms and being able to identify who is at risk can help to prevent them in the first place.
What are the causes of hypoglycaemia?
People with diabetes on insulin therapy and/or tablets e.g. gliclazide:
- missed or a delayed meal or snack
- poor appetite, feeling unwell
- not taken enough carbohydrate at the previous meal
- too much insulin (or diabetes tablets such as Gliclazide)
- more activity than usual (without having extra carbohydrate)
- too much or taken alcohol on an empty stomach
- very hot weather which can increase the speed of absorption of insulin
If someone is having a hypoglycaemic event, the priority is to treat it. Once it is treated and the person is safe, you need to think about what may have caused it so that you can prevent it from happening again.
What are the Symptoms of hypoglycaemia?
- tiredness/lethargy/sleepy
- tingling of the lips
- pale or change in colour
- feeling unusually hungry
- change in mood/behaviour/confusion
- sweating
- palpitations
- slurring of speech
- not responding to questions/commands
- poor coordination and/or unsteady on feet
- feeling light headed/dizzy
Hypoglycaemia may lead to falls, arrhythmias or angina/chest pain and coma if not managed quickly and appropriately.
Management of hypoglycaemia (low blood sugar, less than 4mmol/L)
| MILD Conscious and able to swallow | MODERATE Conscious and able to swallow, but in need of assistance | SEVERE Unconscious and unable to swallow May be fitting |
|---|---|---|
| Step 1 | ||
| Administer 20g of fast-acting glucose Choose 1 of the recommended treatments below: • 6 x dextrose tablets* • 5 large jelly babies • 200mls smooth pure orange juice (small carton) • 60mls Lift juice *can be dissolved in small amount of cold water. | Administer 20g of fast-acting glucose in the form of: • 2 tubes glucose gel (10g glucose per tube) How to administer Squeeze the gel into the mouth between the teeth and gums on the lower inner cheeks. | Ask for help, check airway & Call 999 Administer 1mg of Glucagon intramuscular injection only if trained and competent to do so and if prescribed If unable to administer glucagon, or the resident unresponsive to treatment • Place resident in recovery position until emergency services arrive |
| Step 2 | ||
| Wait 15 minutes before re-checking glucose levels If glucose remains less than 4.0mmols/L, or no physical improvement; REPEAT STEP 1 STEP 1 can be done up to 3 times, BUT if no improvement, or condition deteriorates, CALL 999 for emergency assistance | Blood glucose levels can be re-checked after 10 minutes following glucagon | |
| Step 3 | ||
| When the HYPO has been treated successfully, ALWAYS follow-up with a slower-acting starchy carbohydrate such as: sandwich, medium banana, 2 biscuits, 200mls glass of milk, or meal, if due. When hypo event is resolved document actions. ALWAYS INVESTIGATE THE CAUSE OF HYPO. If no obvious cause, or there has been two or more episodes, contact the GP or, if appropriate, the Community Diabetes Team to review medication. |
||
Remember if the person with diabetes is not improving, you should contact the GP or out of hours’ service if appropriate, or ring 999 for help.
If you are worried that a person with diabetes you are caring for may be at increased risk of hypoglycaemia, you should contact the GP or usual health care professional to review treatment to reduce the risk of hypoglycaemic events.

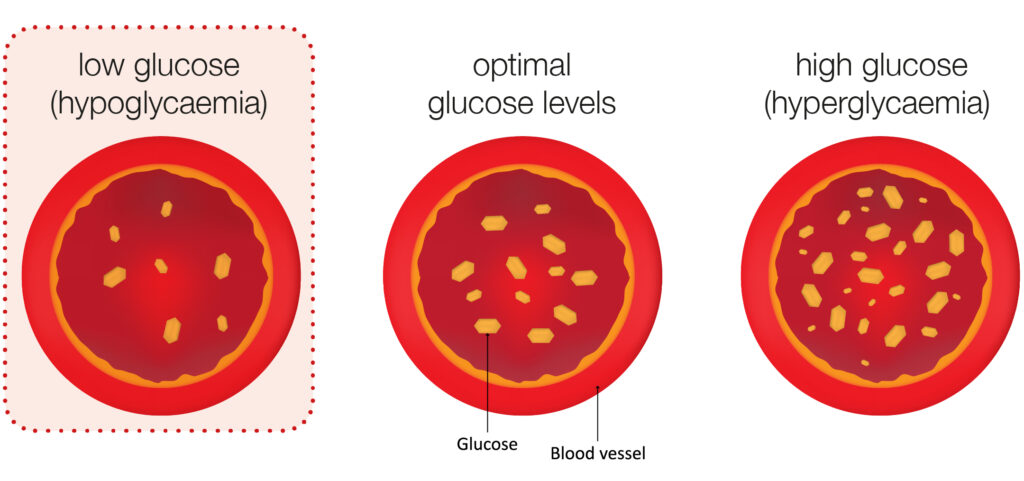
Hyperglycaemia – (high glucose levels)
Hyperglycaemia is the medical term used for high glucose levels. This occurs when the body doesn’t have enough circulating insulin, or the body is resistant to insulin, glucose remains in the blood and cannot enter the cells where it is needed to be used as energy2American Diabetes Association (2020) Approach to individualised glycaemic targets. Arlington County, Virginia, United States: American Diabetes Association.
Why is this important?
High glucose levels can increase the risk of infections and delay the healing process e.g. people will be predisposed to recurring infections despite treatment and if they have a skin condition or a wound this would take much longer to heal and may deteriorate further. Hyperglycaemia can also lead to dry skin and dehydration, which may lead to confusion, delirium or falls.
Persistently raised levels of glucose can lead to many serious life-threatening complications. Therefore, to prevent potential complications it is essential blood glucose levels are managed appropriately3Mouri M; Badireddy M (2021) Hyperglycaemia. NVBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health https://www.ncbi.nlm.nih.gov/books/NBK430900.
If you are caring for someone with diabetes and they have raised glucose levels that are not responding to treatment, you must contact the GP or usual health care professional.
Who is at risk of having hyperglycaemia?
- people with diabetes that are currently unwell particularly if they have a fever or infection
- stress can increase glucose levels
- any changes with their medication
- those who have not had a medication review in some time
- people on steroid therapy
- those with other chronic conditions
- people who are obese, overweight or have had a sudden weight increase
- those who are taking antipsychotic medications e.g. Risperidone, Olanzapine etc.
- those with swallowing difficulties or who may not be able to tolerate their medication
- people who may have poor absorption of insulin due to hard or soft lumps at the injection sites known as lipotrophy
- any changes in their diet and/or activity levels
It is likely that a person with diabetes will experience hyperglycaemia at some point in their life. Therefore, it is vital you are able to recognise and report the symtoms to their health care provider.
An occasional episode of hyperglycaemia should not be a cause of great concern and will often return to normal levels over a course of a few hours with or without treatment.
A client with high blood glucose levels over an extended period needs to be reviewed.
If you are worried, you need to contact the GP in the first instance or their usual health care professional. Alternatively, it may be appropriate to contact the Out of Hours Service.
Cause and Prevention of Hyperglycaemia
Knowing what causes hyperglycaemia will help you to assess someone who may be at an increased risk of developing high glucose levels so that you can try to prevent it in the first place4Diabetes UK (DUK) (2020) Hyperglycaemia (Hyper’s) accessible from: https://www.diabetes.org.uk/guide-to-diabetes/complications/hypers. Think about the following:
- the amount and type of carbohydrate portions eaten – too large may lead to hyperglycaemia
- Encourage appropriate daily activity (discuss with health care professional if unsure)
- Remember diabetes medication should be taken as prescribed and at the right time
- Over treating a hypoglycaemic event (hypo – low blood glucose) could lead to high glucose levels
- Medication reviews are important to ensure they are on the right treatment, making changes where necessary
- Monitor blood glucose levels more frequently unwell
- Encourage sugar free fluids to prevent dehydration
Diabetes UK (DUK) (2020) Hyperglycaemia (Hyper’s) accessible from: https://www.diabetes.org.uk/guide-to-diabetes/complications/hypers
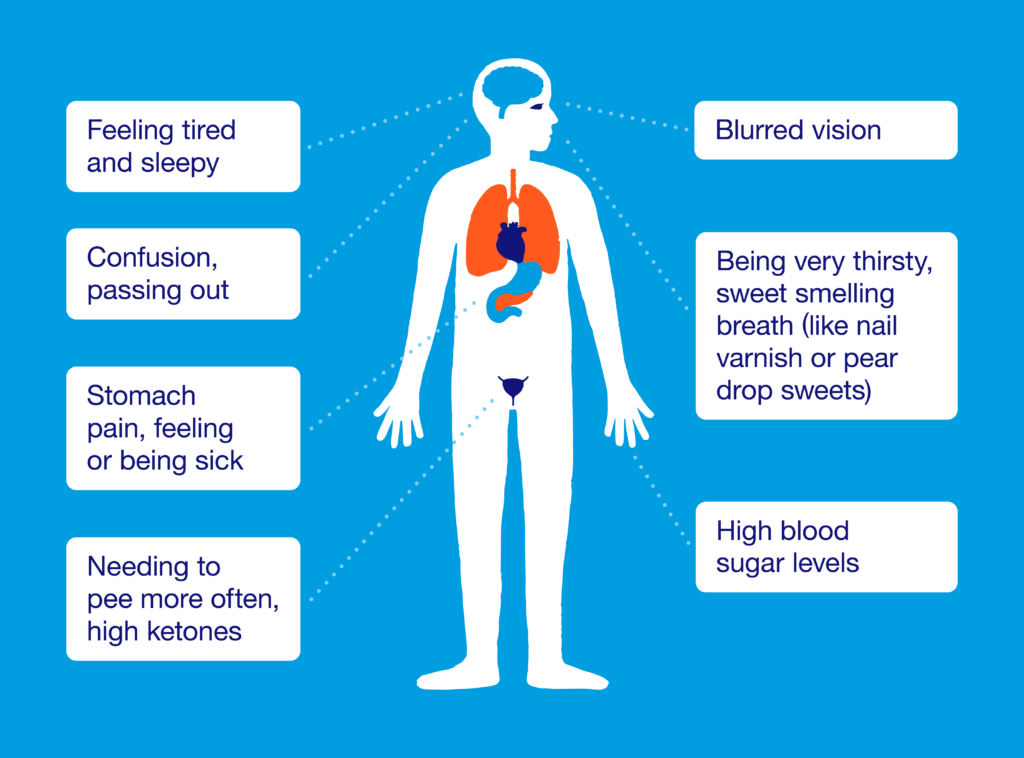
Symptoms of Hyperglycaemia
Diabetes UK (DUK) (2020) 5Hyperglycaemia (Hyper’s) accessible from https://www.diabetes.org.uk/
guide-to-diabetes/complications/hypers
Other symptoms may include
- Incontinence (can often be associated with age) or urgency in trying to go to the toilet
- Dry mouth, dry skin
- Falls particularly if they have poor mobility and are needing to make frequent toilet trips
- Recurrent infections e.g. urine infections; thrush; chest/wound infections; poor healing
- Confusion or in some cases delirium or worsening of dementia and or mental health
If you are worried, you need to contact the GP in the first instance or their usual health care professional. Alternatively, it may be appropriate to contact the Out of Hours Service.
Type 1 diabetes, what to do when you are unwell
Type 2 diabetes, what to do when you are unwell
Acute Complications of Hyperglycaemia
Diabetic Keto-Acidosis (DKA)
When the body doesn’t have enough insulin to allow glucose to enter the cells for energy, the body turns to an alternative source for energy and starts to break down fats.
This produces ketones. Ketones make the blood acidic, this can be extremely dangerous and life threatening.
DKA can happen to anyone with diabetes, but it is more common in type 1 diabetes. Hyperglycaemia is not always present when they develop ketones, but they will be unwell. Therefore, if you are concerned about someone who is unwell you should contact their health care professional.
Diabetes medications e.g. Dapagliflozin, Empagliflozin and Canagliflozin increase the risk of DKA in people with type 2 diabetes. During times of illness these may need to be temporarily stopped. DKA is usually caused by an acute event or underlying infection. Again, if you are concerned about someone with diabetes who is unwell and you suspect they may have DKA, contact their health care professional immediately for advice.
TREND are an excellent resource for guidance on managing diabetes during intercurrent illness:
Hyperosmolar Hyperglycaemic State (HHS)
This can occur in a person (adult) with diagnosed or undiagnosed Type 2 diabetes. They may present with severe dehydration and marked hyperglycaemia (30 mmol/L or more) they will be very unwell. HHS is a medical emergency that requires urgent medical attention6Joint British Diabetes Societies for Inpatient Care Group Diabetes at the front door. A guideline for
dealing with glucose related emergencies at the time of acute hospital admission. February 2020 (internet publication). https://abcd.care/sites/abcd.care/files/site_uploads/JBDS_Diabetes_Front_Door.pdf. It is usually caused by an acute event e.g. heart attack or acute kidney problem but commonly it is due to an underlying infection.
What to do if the person with diabetes is unwell and you suspect DKA or HHS?
There are resources available that provide information on sick day rules – but you should contact the GP or out of hours’ service immediately for advice.
Type 1 diabetes, what to do
when you are unwell
Type 2 diabetes, what to do
when you are unwell
12 Short Term Complications
- 1Adapted with permission from the Diabetes Monitoring Plans for Nursing Homes devised by Nicola Hewer CDSN Education Practitioner C&V UHB 2021, Adapted from A Covid-19 Response Action – Diabetes Management in Care Homes. A National Stakeholders Covid-19 Response Group Interim Guidance. Covid-19 and Diabetes: Interim Care Home Guidance (28th April 2020) National Stakeholders Writing Group and Contributors Professor Alan Sinclair (Co-Chair), Professor Ketan Dhatariya (Co-Chair), Olivia Burr, Dr Dinesh Nagi, Professor Partha Kar, David Jones, Dr Philip Newland-Jones, Dr Kath Higgins, Dr Mayank Patel, Dr Ahmed Abdelhafiz, Dr David Hopkins, Dan Howarth, Catherine Gooday. Accessible from: Covid-19-and-Diabetes-Care-Home-Guidance-28042020.pdf (abcd. care)
- 2American Diabetes Association (2020) Approach to individualised glycaemic targets. Arlington County, Virginia, United States: American Diabetes Association
- 3Mouri M; Badireddy M (2021) Hyperglycaemia. NVBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health https://www.ncbi.nlm.nih.gov/books/NBK430900
- 4Diabetes UK (DUK) (2020) Hyperglycaemia (Hyper’s) accessible from: https://www.diabetes.org.uk/guide-to-diabetes/complications/hypers
- 5Hyperglycaemia (Hyper’s) accessible from https://www.diabetes.org.uk/
guide-to-diabetes/complications/hypers - 6Joint British Diabetes Societies for Inpatient Care Group Diabetes at the front door. A guideline for
dealing with glucose related emergencies at the time of acute hospital admission. February 2020 (internet publication). https://abcd.care/sites/abcd.care/files/site_uploads/JBDS_Diabetes_Front_Door.pdf