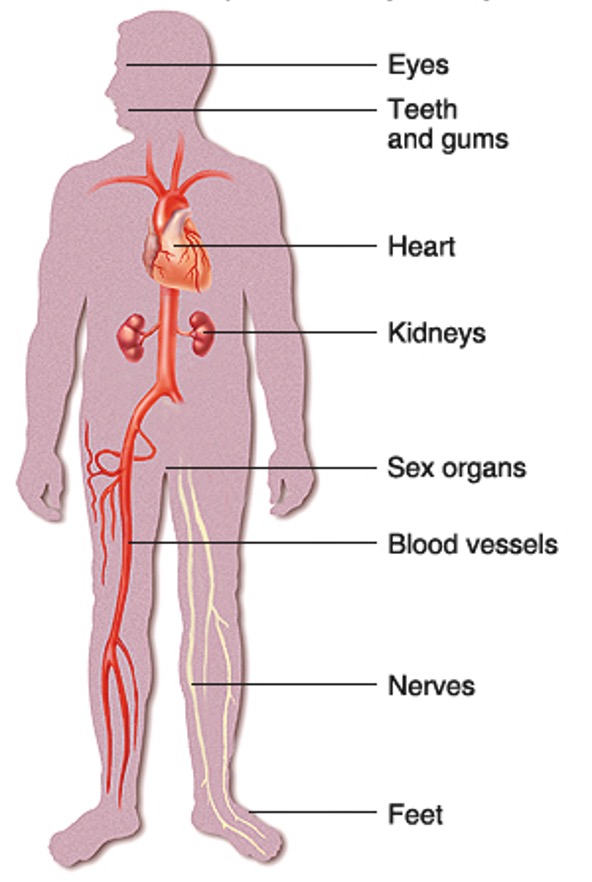
Permanent damage can occur in the body as a direct result of persistently raised blood glucose levels1NICE (2020) Managing blood glucose in adults with type 2 diabetes. Chapter 4 NICE Pathways. London: National Institute for Health and Care Excellence. This is why it is important to try to maintain glucose levels between 6 – 12 mmol/l. Too much glucose in the blood can be very irritant to the blood vessels and can lead to a build-up of fatty deposits in the blood that can damage the blood vessel walls. This can lead to the following complications, or if complications already exist it can accelerate them:
Heart attack, stroke and poor circulation to the big vessels in the legs (peripheral vascular disease)
High glucose levels over a period of time damages blood vessels and this can lead to high blood pressure and poor blood flow. Raised glucose levels in the blood can lead to the development of fatty plaques and these can rupture and form clots. This can sometimes lead to heart attacks, strokes and/ or peripheral vascular disease.
Kidney problems (nephropathy)
Diabetes can cause damage to the kidneys over a long period of time making it harder to clear extra fluid and waste from the body. This is caused by high blood glucose levels and high blood pressure. It is known as diabetic nephropathy or kidney disease.
Nerve damage (neuropathy)
High blood glucose levels may lead to nerve damage. This can make it harder for the nerves to carry messages between the brain and every part of the body so it can affect how we see, hear, feel, move and touch.
Eye problems (retinopathy)
Some people with diabetes develop an eye disease called diabetic retinopathy which can affect their eyesight. If retinopathy is picked up – usually from an eye screening test – it can be treated and sight loss prevented (see section on eye screening).
Foot problems
Having diabetes means people are more at risk of serious foot problems which can lead to ulceration and potential amputation if untreated. Nerve damage can affect the feeling in the feet. Raised blood glucose levels reduces circulation which can lead to poor healing wounds. It is essential to tell the GP if you notice any change in the person’s feet.

Gum disease and other mouth problems
High glucose levels can lead to bacteria in the mouth which can increase the risk of infection in the teeth and gums. The blood vessels in gums can also become damaged, making gums more likely to get infected.

The higher a HbA1c level (glucose level in the blood), the greater risk of developing complications or exacerbating existing complications which may affect quality of life.
Diabetes Annual review
People living with diabetes are entitled to have a diabetes annual review. These may have been delayed as a result of COVID but will be rescheduled. The appointments may not always be in person and may be offered as a video or telephone call instead. People with more urgent needs will be prioritised. Advice to prepare for the appointment is available using the following link: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/preparing-remote-appointments
What can you do to help?
The following care processes should be checked at least annually. This can be done as part of their annual diabetes review. If the person with diabetes is not able to attend for these checks, either in their GP surgery or in their hospital diabetes clinic, then you need to contact their GP and they may be able to arrange to have these checks in the community.
What are the guidelines?
The NICE Clinical Guidelines outline the healthcare checks or care treatment targets for people
with diabaetes. According to these guidelines, every person over 12 years old with diabetes should
receive the following nine healthcare checks at least once a year.
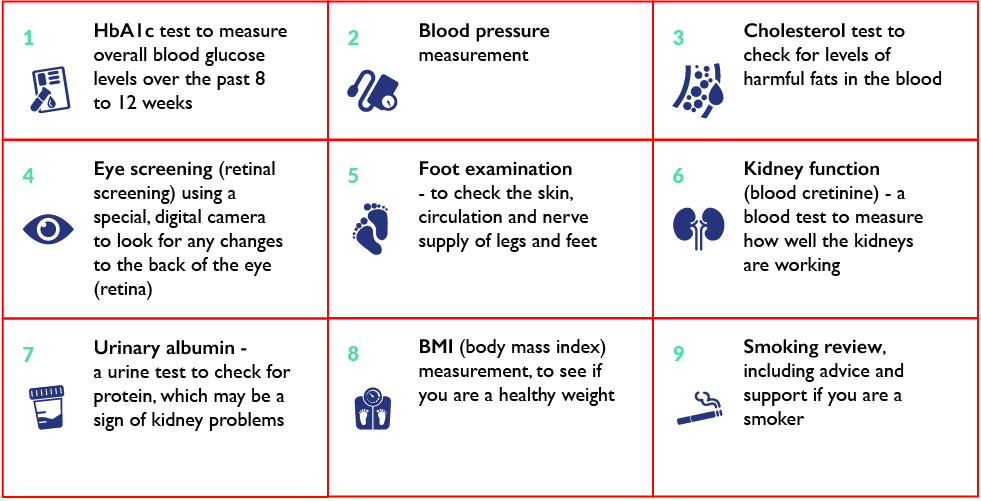
All people living with diabetes should continue to have a diabetes annual review wherever they reside and arrangements can be made with their local health provider to have these checks done if they are unable to access services outside of their home environment.
Elderly people living with diabetes may already have complications of diabetes. However, with good care and managment of risk factors, complications may be prevented altogether, or prevented from getting worse. These are some of the health care essentials that should be reviewed regularly to manage diabetes.
- blood pressure
- fat levels in the blood (lipids e.g. cholesterol levels)
- glucose levels (HbA1c)
- healthy diet
- monitoring weight
- keeping active
- stopping smoking
- care of the feet
- retinal screening
- reducing stress and maintaining emotional health
- medication reviews
- monitoring kidney function
- flu/Pneumonia Covid/Shingle vaccinations
- having annual diabetes review
Complications can in some cases, be prevented, or existing complications may be prevented from getting worse.
Contact the GP if you suspect the person with diabetes may be at risk of any of these complications or if you feel any existing conditions are getting worse
Diabetes UK (2020) have many resources that gives advice on the 15 care essentials that people with diabetes should be receiving to help maintain their health accessible at: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/care-to-expect
Coronavirus (COVID) and Diabetes
People with diabetes who live in care/nursing homes or may be being cared for within their own homes are more vulnerable to the effects of the coronavirus. Due to the level of frailty in this group of people this has resulted in many deaths (Covid-19 and Diabetes: Interim Care Home Guidance 12th May 2020). Poorly managed diabetes can increase a person’s risk of contracting Covid-19 and impact their recovery if they do contract it.
There are many resources and guidance available to help carers support people living with diabetes and these can be accessed from:
https://www.diabetes.org.uk/about_us/news/coronavirus
https://www.diabetes.org.uk/about_us/news/coronavirus-vaccines
COVID-19
Evidence tells us that people with diabetes who contract Covid-19 may be at an increased risk of developing more severe symptoms. It is important that people with diabetes have their diabetes management reviewed.
People living with diabetes are strongly encouraged to have the coronavirus vaccinations
13 Long Term Complications
- 1NICE (2020) Managing blood glucose in adults with type 2 diabetes. Chapter 4 NICE Pathways. London: National Institute for Health and Care Excellence